Press Release: New Survey by The Harris Poll Highlights Gaps in Cervical Cancer Screening Access

FRANKLIN LAKES, N.J., Jan. 10, 2024 /PRNewswire/ -- BD (Becton, Dickinson and Company) (NYSE: BDX), a leading global medical technology company, today announced the results of a Harris Poll survey of women in the U.S., U.K. and Sweden, which shines a spotlight on the differences in access to cervical cancer screening and prevention.
According to the World Health Organization, cervical cancer kills more than 340,000 women globally, every year. It is the fourth most frequent cancer in women, yet it could be virtually eliminated through a comprehensive approach that includes prevention and screening. Human papillomavirus (HPV) is the cause of virtually all cervical precancer and cancer.
Barriers to access
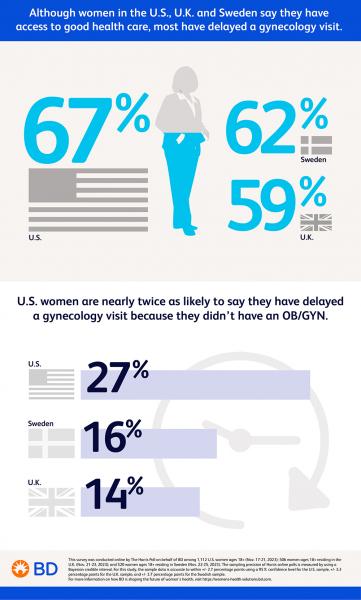
Most women in these countries have delayed a gynecology visit (67% U.S., 62% Sweden, 59% U.K.), primarily due to discomfort with pelvic exams (28% U.S., 38% Sweden) or embarrassment (33% U.K.). Notably, U.S. women are about twice as likely to say they have delayed a gynecology visit because they didn't have an OB/GYN (27% U.S. vs. 16% Sweden, 14% U.K.) or insurance coverage (19% U.S. vs. 8% U.K., 3% Sweden). These results highlight that health equity in the U.S. is lacking, with just 60% of U.S. women reporting that health care in the U.S. provides equal access to all racial and ethnic groups (compared to 79% in Sweden and 76% in the U.K.).
Self-collection for cervical cancer screening is a viable option for increasing access and health equity. It is already available in countries around the world, including Denmark, Sweden, the Netherlands, Kenya, Australia and New Zealand. The study found that the majority of women say they would be comfortable doing a self-collected vaginal test at home to screen for cervical cancer (65% Sweden, 63% U.K., 56% U.S.) and most women (70% U.K., 69% Sweden and 66% U.S.) would be interested in at-home screening for HPV or cervical cancer. Reasons given include being more comfortable in the privacy of their own home, having the ability to administer the test themselves (without a doctor) and not having to make time through an appointment to see a health care practitioner. Notably, younger women are more likely to be interested in self-collection across all three geographies surveyed.
When asked why they might be interested in at-home screening for HPV or cervical cancer, of those interested, women in the U.S. – a country where self-collection is not available -- are twice as likely as women in European countries to want to self-collect at home because it might be less expensive (42% U.S. vs. 25% Sweden, 15% U.K.).
"Self-collection as an additional option could lead to earlier detection of precancer and prevention of cancer," said Nikos Pavlidis, acting president, Diagnostic Solutions at BD. "All women should have access to HPV screening. The U.S. Food and Drug Administration approval of self-collection using HPV testing as the basis for risk stratification would be a first step in the right direction to broaden access in the United States."
Clarity is lacking
Women in the U.K. are more likely to say they are knowledgeable about how often women their age should be screened for cervical cancer (70% vs. 59% US and 44% Sweden), yet the survey found that 36% of U.K. women incorrectly believe that women aged 30-65 need a cervical screening test every year. This awareness gap is more strongly present in the U.S., with 61% whose understanding is incorrect. (In the U.S., the American Cancer Society recommends HPV primary screening for cervical cancer every five years for women aged 25-65.)
Additionally, 73% of Swedish women, 59% of U.S. women and 46% of U.K. women mistakenly believe that Pap (Papanicolaou) tests are the most accurate test for detecting cervical cancer. Most women in the U.S. (65%) know that some types of HPV put women at a higher risk for developing cervical cancer than others, but less than half of U.S. women (49%) recognize that certain ethnicities are more negatively affected by cervical cancer and pre-cancer than others.
"A Pap test looks for existing abnormalities, including cervical precancer or cancer," said Dr. Jeff Andrews, a gynecologist and vice president of medical affairs for Integrated Diagnostic Solutions at BD. "An HPV assay is more sensitive than Pap tests and can identify the potential for abnormalities to develop. When a woman has a positive HPV result, it is important to know what kind of HPV she has—there are different types or strains. The risk of progression varies by type and by duration. And persistence of infection with the same type can be determined with an HPV assay that reports the types."
Education is key
The results showed that most women consider cervical cancer screening a critical part of their health management (86% Sweden, 81% U.K., 76% U.S.). However, many women find the guidance on cervical cancer screening confusing (59% Sweden, 57% U.S., 55% U.K.) and do not understand the difference between a Pap test and an HPV test, despite the fact that HPV is the cause of virtually all cervical cancers. Additionally, women's knowledge about cervical cancer and HPV is lacking, especially in Sweden where only 28% of women consider themselves knowledgeable about cervical cancer screening options, versus 62% of women in U.K. and 59% of women in the U.S.
"As a physician, I have an obligation to educate patients about ways to prevent and options to screen for cervical precancer," said Dr. Andrews. "As patients, women deserve more information on how they are being tested, including the type of test, how often they are being tested and why. Screening techniques advance and guidelines change. My patients are interested in knowing more about HPV, the types, the risks, and management of abnormal results. More knowledge about high-risk HPV types and cervical cancer screening can empower people with a cervix to take greater control of their own health."
This survey was conducted online by The Harris Poll among 1,112 U.S. women ages 18+ (Nov. 17-21, 2023); 506 women ages 18+ residing in the U.K. (Nov. 21-23, 2023); and 520 women ages 18+ residing in Sweden (Nov. 22-25, 2023). The sampling precision of Harris online polls is measured by using a Bayesian credible interval. For this study, the sample data is accurate to within +/- 2.7 percentage points using a 95% confidence level for the U.S. sample, +/- 3.3 percentage points for the U.K. sample, and +/- 3.7 percentage points for the Swedish sample.
For complete research method and additional survey results, please contact mela.sera@bd.com.
About BD
BD is one of the largest global medical technology companies in the world and is advancing the world of health by improving medical discovery, diagnostics and the delivery of care. The company supports the heroes on the frontlines of health care by developing innovative technology, services and solutions that help advance both clinical therapy for patients and clinical process for health care providers. BD and its more than 70,000 employees have a passion and commitment to help enhance the safety and efficiency of clinicians' care delivery process, enable laboratory scientists to accurately detect disease and advance researchers' capabilities to develop the next generation of diagnostics and therapeutics. BD has a presence in virtually every country and partners with organizations around the world to address some of the most challenging global health issues. By working in close collaboration with customers, BD can help enhance outcomes, lower costs, increase efficiencies, improve safety and expand access to health care. For more information on BD, please visit bd.com or connect with us on LinkedIn at www.linkedin.com/company/bd1/, X (formerly Twitter) @BDandCo or Instagram @becton_dickinson.



